The big man with the chainsaw and the gaping wound on his face jumps out from around the corner and growls. You leap backward, your heart pounding in your ears. You’re ready to either take that power tool and teach him a lesson or to run like the kid from Home Alone.
Haunted houses are great examples of stimuli that induce the fight or flight response. The name is suggests two mechanisms are fighting it out, but there is really only one biologic pathway. Whether an animal tries to escape or tries to defend itself, its muscles and mind need to be ready.
In response to a threat, the brain triggers the release of epinephrine and cortisol from your adrenal glands into the blood. As a result, your heart beats faster and stronger, your blood vessels dilate to move more blood, and your lung vessels dilate to exchange more oxygen for carbon dioxide. Equally as important, your liver breaks down glycogen (a sugar storage molecule) to glucose and dumps it into your bloodstream.
All these processes work together to increase your alertness and increase the power of your muscles for a short time - like mothers who lift cars off their small children. You are now ready to respond to the threat; however, there is an exception – you may do nothing at all.
One of the major control mechanisms of the fight or flight response is the autonomic nervous system. This is part of the peripheral nervous system (PNS, outside the brain and spinal cord) and transmits information from the central nervous system to the rest of the body. The autonomic system controls involuntary movements and some of the functions of organs and organ systems.
Parts of the autonomic system acts like a teeter-totter, doing different jobs. It is their relative balance that controls the outcomes. In the fight or flight response, the sympathetic system predominates and your heart rate increases and your blood vessels dilate.
Many people have had the experience of parasympathetic domination coincident to a threat, for some folks it proceeds long enough to have an observable result – they faint. The vagus nerve (a primarily parasympathetic cranial nerve) controls much of this response, so it may be called the vasovagal response. The parasympathetic-mediated reduction in blood oxygen and glucose do not spare the brain - and when your brain is starved of oxygen and glucose, you pass out. Fighting or fleeing is difficult when you are unconscious.
Lower animals will faint as well, but they have additional defenses along these lines. Mammals, amphibians, insects and even fish can be scared enough to fake death – ever hears of playin’ opossum?
There are overlapping mechanisms for feigned death, from tonic immobility (not moving) to thanatosis (thanat = death, and osis= condition of, playing dead). When opossums employ thanatosis, they fall down, stick their tongue out, and even emit a foul smelling odor from glands around their anus. One study in crickets showed that those who feigned death the longest were more likely to avoid being attacked, so this is definitely a survival adaptation – except for the opossums scared by cars and decide to play dead in the street.
Feigned death deters predation, so being scared ain’t all bad. Many predators won’t eat something that is already dead, so not moving could protect them from attack. Another theory is the clot formation hypothesis; it contends that slowing the heart and blood flow forces blood clots to form faster. This will reduce the amount of blood lost during an attack, improving chances for survival.
New evidence is suggesting that even humans undergo tonic immobility. Post-traumatic stress patients asked to relive their trauma show definite signs of tonic immobility, although first they show signs of "attentive immobility," which is more voluntary then the tonic form.
In their new book, Zoobiquity, What animals can teach us about health and the science of healing, Barabara Natterson-Horowitz and Kathyrn Bowers talk about capture myopathy in animals. Small traps that limit movement, cause pain, or are associated with loud noises can cause spontaneous death in live-trapped animals. Several decades ago it was not unusual for 10% of trapped animals to die. In birds, the death rate often rose to 50%! More humane methods of live trapping have reduced the death rate, but point is made – these animals were scared to death.
A human analogy of capture myopathy may have been identified. People that have had a sudden emotional shock, perhaps the death of a loved one, some other tragic occurrence, or crippling fear can undergo something that looks a lot like a heart attack, even if they have no history of heart disease.
This sudden loss of heart rhythm has been called broken-heart syndrome, but is more accurately termed stress cardiomyopathy (SCM). In these cases, the heart actually changes shape! The part of the heart that pumps blood out to the body (left ventricle) balloons out and loses the ability to pump efficiently. Dramatically less efficient pumping leads to symptoms just like a heart attack.
I was wondering if there was a link between SCM in humans and capture myopathy in animals, so I asked Dr. Natterson-Horowitz. She told me that those studies have not been done yet; we don’t know if there is a heart shape change in captured animals. I think it would be hard to get approval for studies that would intentionally scare animals to death.
One interesting connection amongst fight or flight, capture myopathy, and SCM is the catecholamine dump involved. Epinephrine and norepinephrine control all three responses, and in humans, they control even more. Recent evidence shows that catecholamines mediate the production of fear memories.
You remember fearful events more readily and more vividly as a survival adaptation. Strong memories help you to avoid dangerous situations in the future. In this way, your mind can affect how your body responds to a threat. We will see this again in just a bit.
You remember fearful events more readily and more vividly as a survival adaptation. Strong memories help you to avoid dangerous situations in the future. In this way, your mind can affect how your body responds to a threat. We will see this again in just a bit.
The startle reflex involves squinting to protect the eyes, raising the arms, hunching the body to protect the back of the neck, as well as inducing the fight or flight response. With the loss of inhibitory signaling, the signals that ramp up a startle response are unchecked and can lead to uncontrolled beating of the heart (ventricular fibrillation, VF) and sudden cardiac death.
Just as some cases of the fight or flight response going too far, the startle can sometimes lead to VF. A recent study has shown that the bigger the perceived threat, the bigger the startle reflex will be. Also, if there is a fearful environment prior to the threat, then the startle will be bigger. Once in a long while, it goes too far.
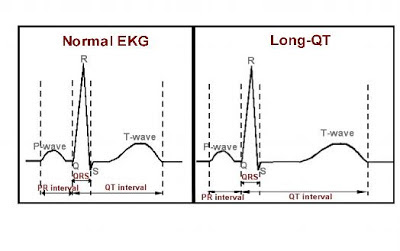
Similar to hyperekplexia, there is another condition that could lead to VF and death in the environment of fear. Long QT syndrome can either be inherited or acquired later in life, and affects the time between beats of the heart. In long QT, the interval is variable and longer, and can lead to inefficient beating and VF.
Last weekwe talked about premature burial. It would be easy to envision a person waking up inside a coffin, and then dying from the fright of being buried alive! Does this mean that you are putting yourself in peril every time you visit a haunted house at Halloween? Probably not, remember that deaths from fright are exceedingly rare. Maybe you could just feign death, and the horrible monster will leave you alone.
Next week, something less macabre. Let’s look at the biology of two Halloween staples - jack o’ lanterns and candy corn.
Greek, R. (2012). Zoobiquity: What Animals Can Teach Us About Health and the Science of Healing. By Barbara Natterson-Horowitz and Kathryn Bowers. Knopf Doubleday Publishing: New York, NY, USA, 2012; Hardback, 320 pp; $16.23; ISBN-10: 0307593487 Animals, 2 (4), 559-563 DOI: 10.3390/ani2040559
Volchan, E., Souza, G., Franklin, C., Norte, C., Rocha-Rego, V., Oliveira, J., David, I., Mendlowicz, M., Coutinho, E., Fiszman, A., Berger, W., Marques-Portella, C., & Figueira, I. (2011). Is there tonic immobility in humans? Biological evidence from victims of traumatic stress Biological Psychology, 88 (1), 13-19 DOI: 10.1016/j.biopsycho.2011.06.002
For more information or classroom activities, see:
Fight or flight –
Autonomic nervous system –
Thantosis/tonic immobility –
Stress cardiomyopathy –
Hyperekplexia –
Long QT syndrome -