Biology concepts – chimeras, microchimerism, autoimmunity, tolerance, self, rejection, graft vs. host disease, HLA, Rh factor
We all know about the dangers of organ transplant; the replacement organ isn’t yours, so your body might try to destroy it (immune rejection). Your cells have human leukocyte antigen (HLA) proteins in a pattern that identifies you; cells with a different pattern of HLAs is non-self and will be attacked by your immune system (see this post).
In order to reduce the chance of organ rejection, doctors look for a donor that has similar HLAs to the recipient. You have six different HLA proteins on each cell (A, B, C, DP, DQ, DR). For just A, B, and C, you have over 25 billion possible combinations, although some are rare and some are much more common.
The take home message is that the closer the match between donor and recipient, the less chance there will be of rejection. Over time, science has found out that A, B and DR are the most important for organ rejection – of course you have two alleles of each, one from mom and one from dad, so it can still be tough to find a six antigen match.
For two siblings, there is a 50% chance that they will have three alleles (antigens) match, and a 25% chance that all or none will match. For a non-related donor, a six-antigen match is about 1 in 100,000. Of course, nothing is guaranteed; six antigen matches have been rejected, while some zero antigen matches have worked out perfectly.
Now let’s try to mesh our discussion of rejection and GVHD with what we talked about last week – some dizygotic twins carry cells from each other; they are chimerics. Dizygotic (DZ) twins are no more related to each other than any two siblings, and they often can’t donate organs for one another. So, why doesn't a chimeric person reject some of his/her own cells, just like in rejection or GVHD?
We talked about many cases of people with different genetic profile cells in their body – this would mean they had different HLA profiles as well, yet they're not rejecting each other. There must be more to it.
Just when does a body decides what is self and what is non-self is important in why chimerics don’t attack, or are attacked by, their twin’s cells. The fetus starts to develop T lymphocytes around 14 weeks of gestation and this is much after the formation of chimeras.
The immune system develops tolerance to self over time, and a chimera has different cells before tolerance is determined. The developing fetus sees the chimeric cells as self. But can you think of a situation where the organism already has decided what is self and then cells with a different profile show up? It’s a lot like a transplant, but it’s naturally occurring. The answer - pregnancy.
This is especially dangerous in the next pregnancy, if that next baby is also Rh+. The mom has been sensitized and antibodies will cross the placenta and attack the baby’s RBCs. Mom is given RhIg (anti-anti-Rh antibodies; think about it) to bind up her anti-Rh antibodies and keep them from attacking the baby. Yes, antibodies cross the placenta; that’s how babies have a bit of immunity immediately after they are born. They start to make their own antibodies about 3-6 months after delivery (except IgM, they make a little of this in the womb).
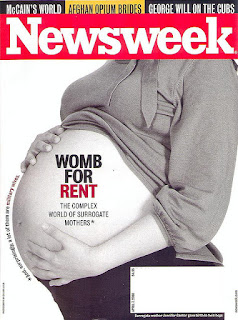
Most people believe that the placenta is a barrier that keeps all the mom’s immune cells (not just the Rh recognizing ones) from attacking the genetically different baby. And to a certain extent this is correct. The placenta is an immune privilegedsite. Most things don’t get through and this protects the baby from the mom’s immune system. It works well enough that some women can choose to be a gestational surrogate– an egg from a different mom, fertilized with a male gamete, is transferred to her and she carries the baby to delivery. The baby is nothing like her genetically, but the pregnancy most often goes off without a hitch.
In just about every pregnancy (maybe every one) some of mom’s cells end up n the fetus and some of the fetus’ cells end up in mom. The number is low, less than 1% of the baby’s cells will be genetically mom’s, so it is called microchimerism.
Some of the cells that get through are likely to be stem cells, and since we can find them in people many years later, they must take up residence and live there – this isn’t like getting a blood transfusion and having a few cells that are different genetically for just a short time. The cells can live there at least 40 years (probably longer). There are different types of microchimerism, depending on where the cells come from and where they end up, and they might have a big impact on health. Let’s look at the types –
Fetal Cell Microchimerism (FCM) – It is a well known fact that women who give birth are less likely to have breast cancer. The reasons for this are a bit up in the air, but one hypothesis is that reproductive hormones increase your chance of breast cancer, and women who have had a baby had an interruption of those hormone cycles while they carried the baby. This reduces their overall chance (breast feeding prolongs the disruption, so it might reduce chances even more).
 |
The easiest way to discover microchimerism? Look for a Y chromosome in women who have given birth to boys (X on the left, Y on the right). One recent study found Y DNA in a new mom’s brain! And microchimerism may mean something. A 2014 study found higher FCM in mom leads to longer survival – less cancer and less heart disease. |
There may be other effects as well. The first studies on FCM and mom’s health were done while investigating scleroderma, an autoimmune disease. Scleroderma hits more post-menopausal women, after they have had kids. Early studies found that women with scleroderma were more likely to have higher levels of FCM, and they found that the fetal cells were often in the skin, where scleroderma strikes.
So, is FCM helping or hurting mom? A later study stated that FCM might actually protect mom from scleroderma, but that if the women had cells from their own mothersthey were more likely to contract scleroderma. And a newer study of maternal thyroid autoimmune disease found that the healthy controls had more FCM than in women with Grave’s disease or Hashimoto’s thyroiditis. The fetal cells were also more likely to be in the vessels and the thyroid follicle cells. Are they there to repair damage from the immune system? Or to induce more tolerance?
Maternal microchimerism(MMc) - Yes, you read that correctly above, babies (even when grown up and are moms themselves) can harbor cells from their mothers. In some babies, this may not work out so well. It may be why they end up with juvenile (type I) diabetes, since some studies show kids with diabetes have more MMc.
Mom’s stem cells might infiltrate the pancreas and differentiate to become the islet cells that make insulin. This may induce an immune reaction to mom’s cells which then, through molecular mimicry(one looks enough like the other), switches to an attack on the baby's own islet cells. It can’t just be from attacking the mom’s cells as islets because not every islet cell is from mom – there must be a switch in the attack to cells that look similar.
 |
A 2014 study says that while FCM should promote fitness in the baby and MMc should promote mom’s fitness, but there can also be issues when it comes to limited resources and sibling rivalry. More FCM could put off another pregnancy and keep more food for the first baby. There be more as well in tying the mother more to one offspring than the other. |
Maternal Transfer Microchimerism– This is the weird one. Imagine cells transferred from baby to mom. Then later mom gets pregnant again, and some of the cells of the first baby end up in the second baby. Now the siblings are microchimeras to each other. One study showed that DZ twins with two placentas and two amniotic sacs still had cells from one another – they must have been passed through the mother.
Another study showed a woman who had not given birth had cells of different profile, but not her mom’s cells; they were from an older sibling. The cells must have moved from sibling to mom to her. And yet another paper found male (XY) cells in umbilical blood of female child – they could only have gotten there by transmaternal passage. Are we all carrying cells from somebody else??
Next week – the weirdness of DZ twins continues. Just what determines if two babies are twins? Over the next three posts we'll see that no decent definition exists.
For more information or classroom activities, see:
HLA system –
Rh factor –
Microchimerism -