Biology concepts - hygiene hypothesis, immune regulation, bacterial drug resistance
Is everyone their own worst enemy? Google it---- apparently scientists are their own worst enemy; Christians are too. Chad Johnson is, and so was Whitney Houston. Someone out there even thinks bassists are their own worst enemies! I think that if this is true, everyone must be leading pretty lucky lives; the only thing stopping us appears to be us.
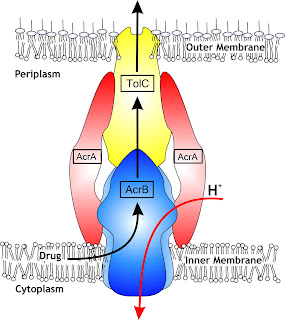
In a situation where an organism is exposed to low or medium levels of triclosan, the multidrug efflux pump actually becomes more active because the triclosan binds to, and suppresses, the pump’s off switch. Think about that - you’re taking an antibiotic for a respiratory infection. But your household products are contaminating your body with triclosan. As a result, the respiratory organism is very efficiently expelling the antibiotics you are taking! Now the bacteria are being exposed to lower levels of antibiotic and will have a better shot at developing resistance! Perhaps anti-bacterials aren’t such a great idea.
our health.
Then again, increased immune hypersensitivity in at risk populations might be due to an imbalance between the innate and adaptive immune systems. Many of the microbiologic antigens to which neonates and children need exposure stimulate innate immune receptors. The innate immune system then stimulates the adaptive immune system and balances the Th1 and Th2 responses. An absence of innate immune stimulation leaves the adaptive system to its own devices, and Th2 will often win this battle.
The hygiene hypothesis can be expanded to test the idea that farm kids' exposure to farm milk and cowshed dust (big sources of arabinogalactan) stems allergy and asthma development. However, there are studies that do not support the hygiene hypothesis, such as influenza virus actually promoting the development of asthma and the fact that daycare children have more respiratory infections, but do not have lower incidence of allergy. More needs to be known before we start shipping our infants to the country for the summer.
Gennady Cherednichenkoa, Rui Zhanga, Roger A. Bannisterb,Valeriy Timofeyevc, Ning Lic, Erika B. Fritscha, Wei Fenga, Genaro C. Barrientosa, Nils H. Schebbd, Bruce D. Hammockd, Kurt G. Beame, Nipavan Chiamvimonvatc, and Isaac N. Pessaha (2012). Triclosan impairs excitation–contraction coupling and Ca2+ dynamics in striated muscle PNAS DOI: 10.1073/pnas.1211314109
So it comes as no surprise that some scientists believe that people are their own worst enemies when it comes to protecting their health. Good intentions can have bad results. How might this relate to our topic of the past few weeks, the benefits of disease and infection?
Some diseases have had a positive effect on survival in specific conditions (like hemochromatosis and plague) and even how malarial fever can kill bacteria. This goes against the popular idea that less disease is better, and that whatever we do to kill infectious organisms is good. We try to be as sterile as possible; just look at what surgeons do before entering the operating room. The health industry has given us antibacterial soaps, cleaning products, plastics, cosmetics, toothpastes, pencils, and even antibacterial computer keyboards!
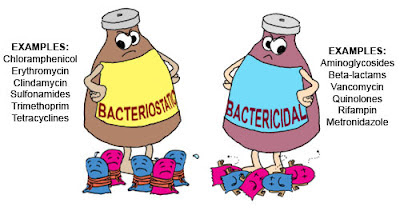
The majority of these products use triclosan as the active ingredient. First introduced as a pesticide in 1972, triclosan (chemical name: 2,4,4’-trichloro-2’-hydroxydiphenyl ether) is an antibacterial and antifungal agent. Triclosan’s mechanism of action at low concentrations is to disrupt fatty acid synthesis as a bacteriostatic agent (slows bacterial growth and reproduction); at high levels it can disrupt membranes and act as a biocidal agent (kills organisms).
Triclosancan control bacterial contamination on hands and skin; hospital staff are encouraged to bathe or shower in triclosan solutions to prevent the spread of MRSA (pronounced “mersa” – methicillin resistant Staphylococcus aureus) in hospital wards. However, this is for control of contamination, not necessarily infection.
Triclosan has been proven effective in reducing infections rates only in cases of gingivitis (inflammation of the gums). However, a 2009 study stated that 75% of Americans over the age of six years have detectable levels of triclosan in their urine. This is significant since there is emerging data that suggests that triclosan might be harmful to people’s health.
High triclosan levels in urine and the environment mean high levels around microorganisms as well. But this shouldn’t be bad – it is supposed to kill germs, isn’t it? Many scientists worry that high triclosan levels also promotes bacterial evolution, selecting for the mutants that are resistant to the chemical. We all have good reason to worry about this because it’s happened before. Many bacteria, from MRSA to Mycobacterium tuberculosis, to vancomycin-resistant enterococcus, are wreaking havoc because we have fewer drugs that are effective against them.
In the laboratory, triclosan exposure has resulted in resistant strains of E. coli, salmonella, and rhodospirillium, and other organisms. Industry scientists argue that there is no data that triclosan causes resistance to develop in the wild, but a 2011 EU report suggests that this very well may be taking place; the levels of triclosan seen in people and the environment are similar to the levels used to drive resistance in the laboratory.
The bacterial resistance mechanism at work might be more dangerous than the resistance to triclosan itself. Several studies have deduced that triclosan interacts with proteins in the bacterial multidrug efflux pump. Many prokaryotes have this system; it works to pump non-bacterial small molecules, including antibiotics and toxins, out of the cell.
Want more evidence? An August 2012 study showed that triclosan has an immediate and dangerous affect on muscle activity. You remember your heart?- it’s a muscle. In mice, triclosan exposure caused a 25% reduction in cardiac muscle function, and an 18% reduction in mouse grip strength. An idea for your next arm wrestling contest – wear a glove and slather it with liquid hand soap. You now have an 18% better chance at winning….if you are competing against a mouse.
Triclosan also affects endocrine function. A new study indicates that triclosan exposure in pregnant rats lowers mother, fetal, and neonatal levels of thyroid hormone. Triclosan has a structure similar to a thyroid hormone; it may trick the body into believing it has enough hormone. The thyroid would then reduce the production of the hormone, leaving the system starved of thyroid hormone. Most of this work has been done in amphibians, fish and rats, but a similar affect on human thyroid function is predicted.
Case in point - most everyone has an idea that food allergies and asthma seem to be on the rise. The CDC stated in 2008 that there had been a 20% increase in food allergies in the years between 1997 and 2007. In a large number of these cases, children with food allergies also had eczema or skin allergies (27%) or respiratory allergies (30%), compared to only 8-9% of kids without food allergies. Basically, allergies are significantly on the rise, and if you have one, you are much more likely to have more than one.
Importantly, the rise isn’t occurring everywhere. Rural Africa - no increase in allergies or asthma. The arctic inuit peoples – very little allergy or asthma despite high levels of childhood smoking. Farm kids in just about every country – far lower levels of respiratory allergies, food allergies, asthma, and autoimmune diseases.
The hygiene hypothesis states that a lack of immune stimulation when young leads to exuberant responses to antigens that would normally be innocuous. Isn’t it interesting that the increase in allergies and asthma also correlates with the onset of antimicrobial agents being added to everything?
Different ideas abound as to how being clean might lead to increased immune hypersensitivities. One hypothesis is that a lack of antigen exposure in urban kids leads to a loss of balance between different T lymphocyte responses (see picture above). Infections tend to stimulate Th1 responses. A too clean, urban environment results in less stimulation of Th1 and therefore a relative over stimulation of the Th2 response. Increased Th2 leads to the kinds of responses seen in asthma and allergies. Indeed, atopic (allergy) patients do show an increase in Th2-driven cytokines.
Additionally, the exposure to bacteria, viruses and parasites stimulates the immune regulatory system as well. Antigen presentation can be stimulatory or suppressive; suppressive presentation leads to regulatory (suppressive) lymphocyte production. It is hypothesized that regulatory lymphocytes help to balance the Th1 and Th2 responses and reduce the incidence of allergy.
We see that several portions of the immune system could be involved in helping the natural environment fine tune our immune responses. But what is it that induces this wonderful balance and state of good health?
A 2010 study suggested that the important molecule is something called arabinogalactan. This is a ubiquitous polysaccharide made of arabinose and galactose monomers. It is a component of many cell walls – bacterial, parasite, worm, grasses and other plants, and is in farm (unprocessed) milk.
Two final notes to bring this full circle. Triclosan use has now been linked to higher rates of allergy. In particular, urinary triclosan levels correlate with development of food allergy. Correlation does not equal cause and effect, but it does ask a question that needs to be answered.
Lastly, increases in autism parallel increases in asthma and allergy, and a recent study shows that kids with autism and behavioral fluctuations have less stimulation of regulatory immune response after infection. Like allergy and asthma, autism definitely has a genetic component, but could the hygiene hypothesis and autism be linked as well?
With Halloween approaching, let's take a three week break from our "disease benefits" stories to look at the biology of some of our Halloween traditions and myths.
For more information or classroom activities, see:
Anti-microbial products –
Triclosan and health –
Hygiene hypothesis –