Biology concepts – desensitization, habituation, counter irritation, cautery, heat sensing, pain, chronic, acute, analgesia
Andreev YA, Kozlov SA, Korolkova YV, Dyachenko IA, Bondarenko DA, Skobtsov DI, Murashev AN, Kotova PD, Rogachevskaja OA, Kabanova NV, Kolesnikov SS, & Grishin EV (2013). Polypeptide modulators of TRPV1 produce analgesia without hyperthermia. Marine drugs, 11 (12), 5100-15 PMID: 24351908
Tobaldini G, de Siqueira BA, Lima MM, Tambeli CH, & Fischer L (2014). Ascending nociceptive control contributes to the anti-nociceptive effect of acupuncture in a rat model of acute pain. The journal of pain : official journal of the American Pain Society PMID: 24412800
Lee MG, Huh BK, Choi SS, Lee DK, Lim BG, & Lee M (2012). The effect of epidural resiniferatoxin in the neuropathic pain rat model. Pain physician, 15 (4), 287-96 PMID: 22828682
Kelly S, Chapman RJ, Woodhams S, Sagar DR, Turner J, Burston JJ, Bullock C, Paton K, Huang J, Wong A, McWilliams DF, Okine BN, Barrett DA, Hathway GJ, Walsh DA, & Chapman V (2013). Increased function of pronociceptive TRPV1 at the level of the joint in a rat model of osteoarthritis pain. Annals of the rheumatic diseases PMID: 24152419
Before adequate drugs and diet suggestions came along to help to rid the body of excess urates, people were sometimes left to to their own devices in trying to relieve the pain of gout. One home remedy was described in a history text from the 500’s CE called Historium Libri Decem.
In the book, the Bishop of Cahors had gout so bad that he would stick a fireplace poker in the embers and then apply it to his foot and shin. Man oh man, it must be some major discomfort if cauterizing your toes and foot becomes a good idea.
The practice of cautery(from Greek for branding iron) for gout lasted for hundreds of years, with a 17th century century surgeon from France pronouncing that he didn’t really believe in external remedies for gout, except of course, for cautery with a red hot poker.
The above example falls under the heading of analgesia (an = not, and gesia = pain) by counter irritation. Counter irritants basically substitute one pain for another. You have two competing stimuli, both of which create pain. One is probably chronic (long-term, comes from chronus = time); this is pain from which the person wants relief.
The second pain is acute(from Greek for sharp). The second pain is geared toward relieving the first pain. Who hasn’t bitten a knuckle or lip while getting an injection or experiencing some other pain? Is it just a distraction, a placebo, or is there biology at work?
The concept of counter-irritation is old. Before we had any idea how it worked or even if it worked, counter irritant uses approached the bizarre. Heart attack and angina pectoris (pain from partially blocked cardiac vessels) often shoot a pain down the left arm. So early physicians decided that if counter irritants were placed on the left arm, they could short circuit the pain as it was sent out but before it could come back to the heart.
Originally used to promote healing, cups are used to quell pain too. As far as truly scientific studies, the only thing we know about cupping and pain relief is that the studies have been poorly conducted – better studies are needed. But never underestimate the power of the placebo. If a patient thinks it works, then it works.
Other types of counter irritants include scarification– scratching until the epidermis is removed. Many people with chronic itch practice this everyday of their lives. Chemical irritants that act on the skin are called rubefacients because they turn the skin red (through dilation of blood vessels underneath). Capsaicin, menthol, camphor, methylsalicylate (more on this below), eucalyptus oil, all have been tried as rubefacient counter-irritants.
A study from 2009 showed you could counter a long-standing pain in the right leg by immersing your leftfoot in cold water. Painfully cold water activates TRPM8 and TRPA1. Doing this only to the left foot reduced shock pain in the right leg by 50%. Apparently it acts to confuse pain signals at the level of the spinal column.
So just how does counter irritation relieve pain? There are competing ideas. Perhaps the acute pain of the irritant sparks a release of endorphins (opiate pain killer made by our own body). This seems plausible, but chronic pain patients have very high levels of endorphins in their blood; they just seem to not respond to them.
The hypothesis of a nerve overload is less precise, and may actually reflect other mechanisms at work. Overload in general would mean that a huge amount of neural input at the same time overloads the spinal nerves at that point and results in no signals getting through. This may be how the left foot right leg example works.
Even if some of these mechanisms contribute to counterirritant action, additional processes are probably at work as well, namely desensitization and habituation. You’ll be surprised how much TRPV1 heat/capsaicin sensors are involved. Capsaicin causes pain because your body interprets it as noxious heat (TRPV1), but somehow, you can also use capsaicin to take away pain.
In simple terms, desensitization of the TRPV1 channels means that while some activation causes pain, continued activation depletes the neuron of the molecules need to create or transmit the signal, and the pain neuron can’t fire any longer. If it can’t fire, there’s no pain – analgesia.
There are two kinds of desensitization, homologous means that continued use of one agonist on a receptor makes that receptor less able to respond to that agonist. Heterologous desensitization is when other agonists work on receptors in another part of the tissue.
The heterologoustype of desensitization sounds an awful lot like the example above where really cold water on one foot reduces pain in the other foot. So this could be one of the mechanisms of counter irritants.
On the other hand, consider the old example of placing a frog in hot water (video here) – it jumps out due to TRPV1 heat/pain signaling. But if you place a frog in warm water and then heat it slowly, the frog won’t jump out. It will sit there until it’s a frog leg dinner. This is habituation (tolerance) and perhaps homologous desensitization as well. Perhaps capsaicin pain creams act by habituation and counter irritation, nothing says they can’t do both.
Another desensitization/habituation model uses resiniferatoxin injected into the covering of the brain (epidura) to stop neuropathic pain. Remember that resinferitoxin is a strong capsaicin-like molecule, with a score of 108.8 billion Scoville units. It is such a strong agonist that it alone can desensitize TRPV1 in short order - so much that it is termed an anti-nociceptive agonist.
Even more amazing, a Sept. 2012 study used two agonists of TRPV1, capsaicin and MRS1477. Use one or the other and you get hyperalgesia. But administer both at the same time and you get analgesia. In this case, they are hoping that this will be an alternative to opiates in cancer-mediated pain.
This all sounds great – TRPV1 is on small (C type) and some larger (Adelta) pain fibers, and wearing them out can reduce pain. But wouldn’t it just be easier to block them with an antagonist (something that binds but doesn’t activate)? Well, there’s a problem with that – TRPV1 does more than just signal pain.
If you block TRPV1 activity to produce analgesia, you also block its heat-sensing role. Now your body won’t know when it is getting hotter and won’t cool itself down. You end up with hyperthermia and that can kill you. This has been a consistent problem with TRPV1 agonists as analgesics, including if resinferitoxin is given orally – but who would want 108.8 billion SHU in their mouth?
It is the oral TRPV1 antagonists that seem to bring the hyperthermia when trying to treat osteoarthritis. The hyperthermia has been attributed to the action of TRPV1 antagonists in the GI tract. New work shows that activity of TRPV1 is increased (and the expression) in the joint during osteoarthritis, but no increase in expression or activity in the spinal column. Injection of a TRPV1 antagonist into the joint to stop the pain signals from the joint without the hyperthermia.
New polypeptides called APHC1 and APHC3 show analgesic activity in vivo at reasonable doses (0.01-0.1 mg/kg) by blocking capsaicin, heat, and acid activation and did not cause hyperthermia.They can be used IV or perhaps orally, they don’t need to be injected into a specific joint or into the spinal column.
Some chemicals may be both agonistic and antagonistic for TRPV1. A new paper states that methyl salicylate (oil of wintergreen) activates TRPV1, so it induces a warm feeling, but it also blocks TRPV1 activation by capsaicin, acid, anandamide, and perhaps inflammatory mediators. This means that it can be analgesic, which is why it's the main ingredient in BenGay.
However, the same paper indicates that analgesic activity of methyl salicylate might be due to its TRPV1-independent activity on a different system, the same pain generating system blocked by aspirin (cyclooxygenase). Arguing against this - BenGay is amazingly painful when loaded into a teammate’s underwear or jock. Take my word for it.
a 2012 study of electroacupuncture showed that it could reduce the size and frequency of the action potentials from TRPV1 nociceptive neurons. To determine how this might work, the same acupuncture point (st36) was shown in a 2014 paper to block pain by stimulating a pain pathway. If you block the anti-nociceptive TRPV1 channels with 1% capsaicin, then the acupuncture won’t stop the pain. Once again, TRPV1 works in both pain and anti-pain. That’s a confusing exception.
Next week, capsaicin receptors are also used in some other systems, not just heat and pain. Who would have guessed that eating chili peppers could stop but also cause cancer?
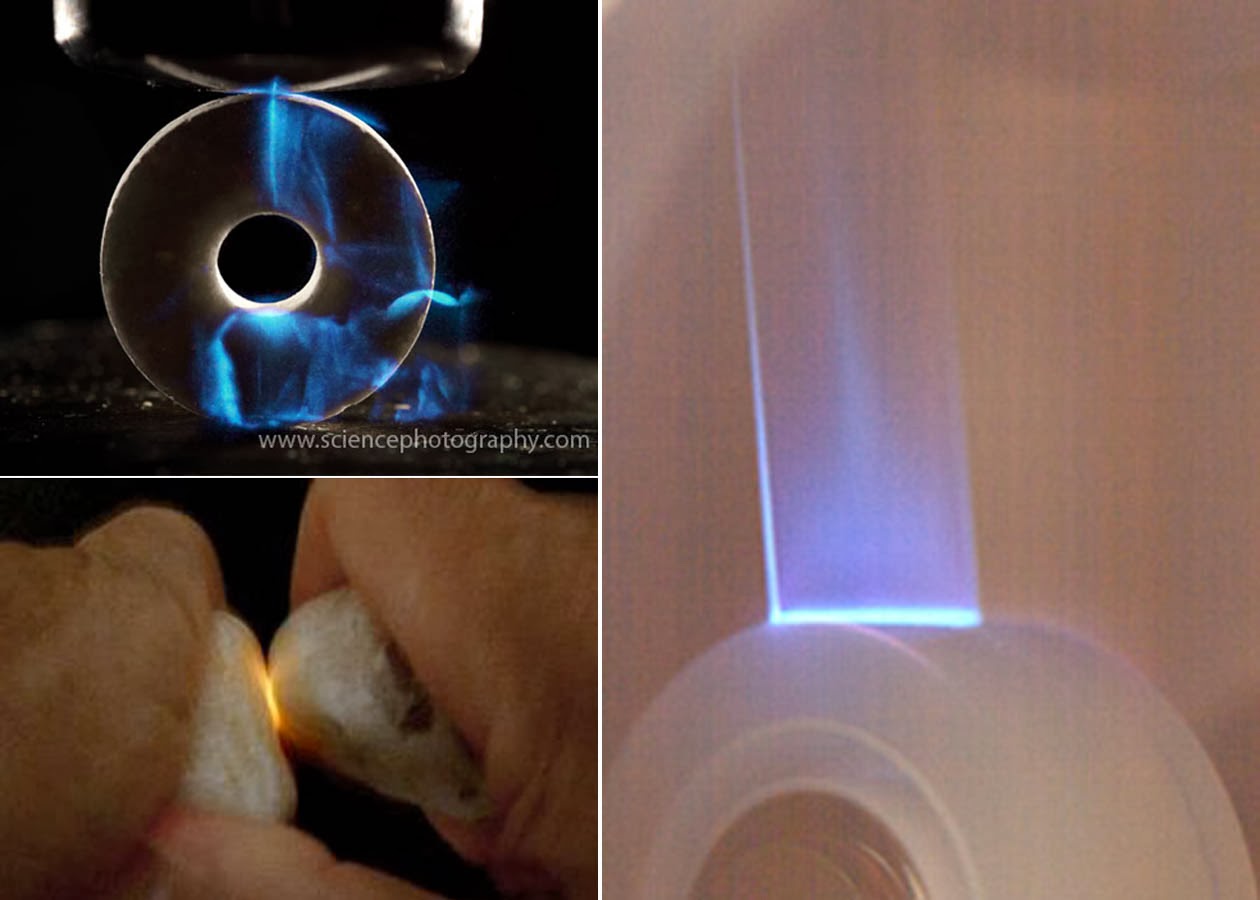
Because pain is involved, I am including demonstration links only for triboluminescence.
For more information, see:
Counter irritants –
Gout –
Acupuncture –
Methyl salicylate triboluminescence –